Medical Orientation
Radiology Result Checking Process
All clinicians check their own results, whether they are the ordering clinician or episode/authorizing care provider. This includes patients that may have been handed over.
All results are expected to be checked within two weeks of the test being completed. The sooner the result is checked, the lower the clinical risk to the patient, and the lower the risk of complaint against the doctor and hospital, because a treatment plan can be put into place more quickly.
If the result is normal, it can be signed off. If there is demonstrated pathology, check the patients notes to ensure that appropriate investigations or treatment were undertaken – if so, sign off the result. If the patient was admitted for that episode of care, it is safe to sign off their result, as the admitting team takes responsibility for the results and follow up once a patient is admitted.
If there is missed pathology (whether it is the primary problem or an incidental finding), depending on your level of training, instigate an investigation and treatment plan or talk to a consultant about an appropriate plan.
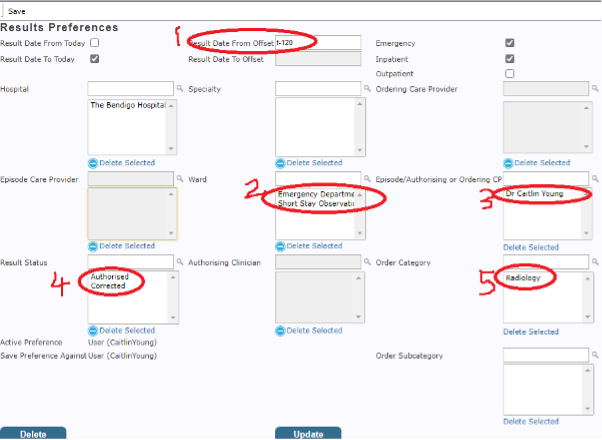
Emergency clinicians should have the following settings on their “unread result tab”
- Result date from: t-120
- Ward: Emergency Department AND Short Stay Observation Unit
- Episode/Authorizing or Ordering CP: Your name
- Result Status: Authorised AND Corrected
- Order category: Radiology