Clinical Resources
Bendigo SSOU Admission Guidelines
Introduction
Bendigo Health ED runs a 12 bed Short Stay Observation Unit (SSOU). Admission to the SSOU is guided by the ED Streaming Model of Care and is in keeping with the Victorian Department of Health Guidelines for Short Stay Units.
Admission Guidelines
Common conditions suitable for admission to SSOU are listed below. Click on each to see our admission guidelines for each of the diagnoses.
Definition
- Patients presenting with either proven DVT or are awaiting imaging to confirm/ rule out the diagnosis. These patients may be admitted pending investigations or to initiate an appropriate treatment plan and follow-up.
Admission Criteria
- DVT most likely below mid-thigh
- Awaiting imaging
Exclusion criteria
- Negative D-dimer and low pre-test probability excludes the diagnosis
- DVT above the inguinal ligament
- Evidence of pulmonary embolism
- Major comorbidity or complicating social/mobility factors
- Neurovascular compromise
- Upper limb DVT: likely to require admission on confirmation
Investigations
- FBE
- UEC
- Doppler Ultrasound
- Documented weight
- Additional as required: INR if on warfarin
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Enoxoparin (clexane) |
1.5 mg / kg to maximum dose 100mg |
Daily |
SC |
|
Apixaban (CrCl ≥25ml/min) |
10mg |
BD for 7 days then decrease to 5mg BD |
PO |
|
OR Rivaroxaban (CrCl ≥30ml/min) |
15mg |
BD for 21 days then 20mg daily |
PO |
|
Paracetamol |
1g |
4hourly PRN |
PO |
|
Ibuprofen |
400mg |
TDS |
PO |
Specific observations
- Accurate weight for clexane dosage in kg (note maximum dose is 100mg)
Report immediately to medical staff any of the following
- Chest pain – please complete ECG if CP occurring
- SOB
- Decreased Sa02
- Pain not responding to simple analgesia
Discharge Criteria
- Suitable home situation
- Able to mobilise
- Adequate social supports
- Patient education and handout
- Script for appropriate medications if required
Hospital admission criteria
- Inadequate social supports
- Ongoing uncontrolled pain
- Development of PE symptoms
Definition
- Acute pyelonephritis is a bacterial infection causing inflammation of the kidneysand is one of the most common diseases of the kidney.
- Pyelonephritis occurs as a complication of an ascending urinary tract infection (UTI) which spreads from the bladder to the kidneys and their collecting systems.
Admission Criteria
- Clinical features suggestive of acute pyelonephritis
- Flank pain
- Pyuria (urine MCS or FWT with leukocytes +/- nitrates)
- Loin pain
- +/- fever
- +/- nausea and vomiting
- +/- dehydration
Exclusion criteria
- Hypotensive not responding to IV fluids or other signs of severe sepsis
- No FWT or MSU done
- Pregnancy
- Renal insufficiency
- Marked debility
- Co-morbidities
- Known renal tract anomaly or significant pathology e.g. single kidney
- Rental tract stent
- Rena tract obstruction
- Immunocompromised patients
Investigations
- FWT
- Urine MCS
- BHCG urine
- FBE
- UEC
- Additional as required
- Renal USS or CT if abnormal renal function or persistent flank pain
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Paracetamol |
1g |
4hourly PRN |
PO |
|
Ibuprofen |
400mg |
TDS |
PO |
|
Normal Saline or CSL |
100ml |
Repeat PRN |
IV |
|
Oxycodone IR |
5-10mg |
4hrly PRN |
PO |
|
Metoclopramide OR Ondansetron |
10mg 8mg |
8hrly |
IV or PO |
|
Moderate – Severe Disease |
|||
|
Gentamicin |
4-6mg/kg |
Single dose |
IV |
|
Ampicillin |
2g |
6hrly |
IV |
|
Mild disease |
|||
|
Augmentin DF |
875/125mg |
BD |
PO |
Specific observations to be notified to staff
- Notify fall in BP to medical staff
- Notify ongoing vomiting or rigors
Specific management issues
- Second episode of pyelonephritis should have renal tract ultrasound as inpatient
Consultations
- Urology if abnormal renal tract investigations
- Medical admission if symptoms/ patient not clinically improving
Discharge Criteria
- Pain managed by oral analgesia
- Systemic toxicity improved
- Adequate oral intake
- May be discharged to HITH
Hospital admission criteria
- Persisting systemic toxicity
- Signs of sepsis
- Not tolerating oral fluids
- Diagnosis unconfirmed on laboratory findings
Discharge follow-up
- GP
Definition
- Migraine is a type of headache characterized by recurrent attacks of moderate to severe throbbing and pulsating pain on one side of the head
- Migraine similar to previous established clear diagnosis but not responding to usual treatment
Admission Criteria
- Clear diagnosis ie similar recurrent headache in past diagnosed as migraine
- Previous normal CT
- Long established history of migraines
- Required IV hydration
- Requires treatment
Exclusion criteria
- Fevers unless non-CNS focus is found e.g. UTI/ URTI
- Impaired consciousness level (GCS <14)
- New focal neurological deficit
- Sudden onset of headache indicated SAH (please see SAH pathway)
Investigations:
- FBE UEC
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Normal Saline or CSL |
100ml |
Repeat PRN |
IV |
|
Analgesia |
|||
|
Paracetamol |
1g |
4hourly PRN |
PO |
|
Ibuprofen |
400mg |
TDS |
PO |
|
Aspirin OR Aspalgin (with codeine) |
900mg |
6hrly (max dose 2.4g in 24hrs) |
PO |
|
Sumatriptan tablet |
50-100mg |
Once |
PO |
|
Sumatriptan (nasal spray) |
20mg |
Once |
IN |
|
Antiemetics |
|||
|
Metoclopramide |
10mg |
8hrly |
PO/ IV |
|
Ondansetron |
8mg |
8hrly |
SL/ IV |
|
Prochlorperazine |
5-10mg |
8hrly |
PO/ IV |
|
Chlorpromazine (Largactil) infusion |
12.5mg in 1000ml Nsaline |
Over 1hr. can be repeated once |
IV |
Non pharmacological treatment
- Cold packs over the forehead or back of the skull (targeting the supraorbital and greater occipital nerves)
- Hot packs over the neck and shoulders (targeting the innervation of the scalp)
- Neck stretches and self-mobilisation
- Rest in a quiet dark room.
Specific observations
- Report drop in GCS by 1 point
- Headache/ vomiting not controlled with maximal treatment
- Report new onset fever
Discharge Criteria
- Pain-free and controlled by oral analgesia
- Normal hydration
- No vomiting
- Appropriate social supports
- Diagnosis certain
Hospital admission criteria
- Headache not controlled by oral analgesia
- Development of new neurological deficit
- Impaired level of consciousness
- Neurological deficit not resolving
- Uncertain diagnosis
Definition
- Patients presenting with PV bleeding who are <20/40 gestation. These patients may require investigations (including bloods and US scan) and consideration of anti-D treatment (for Rhesus negative mothers).
Admission Criteria
- Calculated gestation <20/40
- PV bleeding with NO PAIN (if pregnancy location not known)
- PV bleeding with mild-moderate pain is acceptable if pregnancy is known to be intrauterine
- Anti-D arranged for women with Rhesus negative blood type PRN
Exclusion criteria
- Significant abdominal pain
- Abnormal vital signs
- High suspicion for ectopic pregnancy
Investigations:
- FBE UEC
- Blood group if unknown
- Early pregnancy ultrasound
- Quantitative BHCG (not required if >10 weeks or previous USS showing foetal HR)
- Urine FWT
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Paracetamol |
1g |
4hourly PRN |
PO |
|
Oxycodone IR |
5-10mg |
4hrly PRN |
PO |
|
Buscopan |
10mg |
8hrly |
PO |
|
Anti-D Immunoglobulin for Rh negative blood group |
250 IU if <12/40 625 IU if >12/40 |
Once |
IM |
|
NO NSAIDS in 1st trimester |
|||
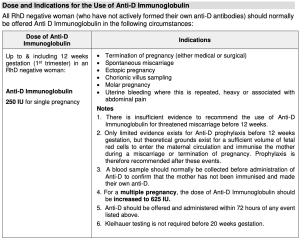
Dose and indications for Anti-D as per RANZCOG guidelines 2022
Specific observations
- Visualize pad changes, if heavy please weigh
- Severe pain
Report immediately to medical staff any of the following
- Excessive PV loss (>1 pad every hour) or passage of products of conception
- Hypotension
- Severe pain not responding to PO analgesia
Consultations
- O&G if miscarriage for management options, on DC for EPAS
Discharge Criteria
- Bleeding settled and pain free with simple analgesia
- USS no concerning features
- Follow-up planned
- Early pregnancy assessment service (EPAS)- needs O&G registrar referral and online request
- Private obstetrician
- GP
Hospital admission criteria
- Persisting pain and bleeding
- Possible ectopic
- Lack of adequate social supports
Definition
- Spontaneous pneumothorax is defined as gas in the pleural space that occurs in the absence of an external event. Spontaneous pneumothorax can be either primary or secondary.
- Primary Spontaneous Pneumothorax (PSP) is a spontaneous pneumothorax that occurs in patients with no underlying lung disease
- Secondary Spontaneous Pneumothorax (SSP) is a spontaneous pneumothorax that occurs in patients with underlying lung disease
- Severity can be defined in terms of size of the pneumothorax as either small or large, and by the patient’s clinical signs and symptoms.
- A small pneumothorax is defined as <2cm distance from the chest wall to the visceral pleural line at the level of the hilum
- Large pneumothorax is defined as a distance of ≥ 2cm from the chest wall to the visceral pleural line at the level of the hilum
Admission Criteria
- Spontaneous pneumothorax
- If secondary size <2cm (small)
- Stable vital signs
- No recent trauma
Exclusion criteria
- Significant hemodynamic instability
- Significant exertional dyspnea
- If secondary Spontaneous pneumothorax large >2cm
- Recurrent spontaneous pneumothorax
- Bilateral spontaneous pneumothorax
- Tension pneumothorax
- Traumatic pneumothorax
- Unstable vital signs
- Chronic lung disease or significant comorbidities
Investigations
- CXR prior to admission
- Repeat CXR at 4-6hours post
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Paracetamol |
1g |
4hourly PRN |
PO |
|
Ibuprofen |
400mg |
TDS |
PO |
|
Oxycodone IR |
5-10mg |
4hrly PRN |
PO |
|
Metoclopramide |
10mg |
8hrly PRN |
PO/ IV |
Specific observations
- Apply supplemental oxygen targets to SpO2 ≥ 96% (88-92% for patient at risk of hypercarbia)
Report immediately to medical staff any of the following
- Report any increasing shortness of breath/ chest pain
Consultation
- AGSU if any deterioration
Discharge Criteria
- Repeat CXR done at 4-6hours indicative of stable or resolving pneumothorax
- Discharging between 8am and 11pm
- Living within 30minutes of the hospital
- Patient is competent.
- Discharge advice (see below) has been provided.
- PSP FU with GP in 2-4 weeks with repeat CXR prior to review
- Patient is able to represent in 12-48 hours for a repeat CXR
Discharge advice
- Patients should be advised to:
- Stop smoking, including cigarettes, other tobacco products, marijuana and illicit drugs
- Avoid any air travel for 1 week post complete resolution of the pneumothorax. An undrained pneumothorax is a definitive contraindication to commercial air travel. A small risk of recurrence up to 1 year after a pneumothorax occurs with any air travel
- Gradually re-introduce exercise after two weeks. Contact sports, heavy weightlifting and extreme exercise may need longer periods of avoidance
- Avoid deep sea diving permanently unless the patient has had a pleurodesis and a normal CT chest
Hospital admission criteria
- Increase in size of pneumothorax on CXR
- Significant symptomatic SOB
Discharge Follow-up
- GP
- Consider surgical OP
- Repeat CXR in 2-4 weeks with GP or to represent to ED if no GP
- Clear education that if worsening SOB to represent to ED
Definition
- Observation and management of the post ictal patient that has not fully recovered in ED
Admission Criteria
- Single seizure in known epileptic or first seizure
- Post 1hr ED observation with improving consciousness state GCS >15
- For observation and short term management
- For IV rehydration
- Requiring anti-convulsant medication level check
Exclusion criteria
- Fever/ sepsis
- Alcoholic withdrawal seizures
- >1 seizure in <24hrs
- Pregnancy
- Head trauma during seizure unless normal CT
- Altered conscious state due to other diagnosis
Investigations
- FBE UEC
- ECG
- BSL
- Optional: Anti-convulsant drug level, CTB, CMP
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Midazolam |
2-5mg |
Stat for seizure |
IV or IM if no IV access |
|
Usual anticonvulsants |
|
|
|
|
OR Levetiracitam |
500mg |
Stat loading |
IV |
Specific observations:
- Watch for repeat generalized seizure
- Note any focal arm/ leg/ facial twitching which may indicate generalized seizure likely to occur
Report immediately to medical staff any of the following
- Repeat seizure
Specific management issues
- Ensure patient usual anti-epileptics medications are charted and given
Consultations
- Austin Epilepsy Registrar (through switch)
- GP/ Physician/ Neurologist who usually manages seizures
Discharge Criteria
- Resolved post ictal state
- Appropriate carer to safe environment
- Advice re swimming, driving, dangerous activities
- EEG and CT (if not already completed)
- Austin 1st Seizure clinic referral- after discussion with Austin Epilepsy Registrar
Hospital admission criteria
- Further seizure
- Persisting low GCS or new neurology
Unable to establish safe environment at home
Definition
- If suspected snake bite only i.e. no clinical or laboratory signs of envenomation and patient not presenting with significant symptoms, then can be managed in SSOU. SSOU consultant must review/ accept patient prior to transfer.
- 90% of bites are dry and contain little to no venom
- Only approximately 5% of snake bites lead to envenomation
- Brown snakes are commonest cause of severe envenoming and fatalities in Australia
Types of snakes and clinical presentation
|
Category |
Venom induced consumptive coagulopathy |
Neurotoxicity |
Myotoxicity |
Other effects |
|
Brown |
Always present with significant envenoming |
Rare |
Not present |
Early collapse (335) or cardiac arrest (3%). Systemic symptoms frequently absent (50%) Thrombotic microangiopathy (10%) |
|
Tiger group |
Always present with significant envenoming |
Uncommon Slow onset over many hours |
Uncommon Slow onset over many hours |
Systemic symptoms common Thrombotic microangiopathy (<5%) |
|
Black |
Not present Mild direct anticoagulant effect. INR/APPT rise but normal fibrinogen |
Not present |
Common Slow onset over hours to days Can result in renal failure |
Systemic symptoms common Local bite site pain and swelling significant |
|
Taipan (uncommon VIC) |
Always present with significant envenoming |
Common may be rapid onset |
Rare |
Systemic symptoms common Thrombotic microangiopathy (5%) |
|
Death adders (uncommon VIC) |
Not present |
Common Slow onset over many hours |
Not present |
Systemic symptoms common Local bite site pain often present |
Admission Criteria
- Snake bite (true or suspected).
- Pressure bandage
- First set of blood tests
- Anti-venom given to patient with signs of
Exclusion criteria
- Significant neurotoxicity (Eg. respiratory distress).
- Post-circulatory collapse / cardiac arrest.
- Haemo-dynamically
- Profuse
Investigations
- Bloods on presentation to ED with pressure immobilization bandage insitu
- If normal and no features of envenomation remove bandage
- Re-apply if any signs of envenomation
- Bloods 1hour post bandage removal
- Can go to SSOU if bloods normal
- Repeat bloods at 6hours and 12 hours post bite
- Bloods
- FBE
- UEC- AKI secondary to rhabdomyolysis or thrombotic microangiography
- Coagulation studies- INR, APTT, fibrinogen
- D-dimer
- CK
- Urine FWT for protein / microglobinuria
- ***Snake venom detection no longer recommended
Evidence of envenomation
- Clinical
- Neurotoxicity- ptosis generally 1st sign, extra-ocular ophthalmoplegia (diplopia), blurred vision
- Myotoxicity- muscle pain and tenderness, weakness, elevated CK
- Coagulopathy – bleeding from gums, IVC site
- Nonspecific symptoms e.g. NV, headaches
- Early CV collapse
- Lab evidence
- INR >1.2
- Prolonged APTT
- Low or undetectable fibrinogen concentration
- Raised D-dimer (at least 10x the assay cut off or >2.5mg/L)
- CK> 1000 units/L
- Raised creatinine
- Evidence of thrombotic microangiography
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Paracetamol |
1g |
4hrly PRN max 4g |
PO |
|
Ibuprofen |
400mg |
6hrly PRN |
PO |
|
Metoclopramide |
10mg |
8hrly PRN |
PO/ IV |
|
Ondansetron |
8mg |
8hrly PRN |
SL / IV |
Specific observations
- Report signs of respiratory
- Report
- Report new neurological symptoms (Eg. ptosis, ophthalmoplegia, limb weakness).
- Report
Specific management issues
- Coagulopathy may not begin to improve until about 12 hours.
- Persistent coagulopathy is not an indication for additional anti-venom.
- Repeat blood tests every 12 hrs until coagulopathy resolved if coagulopathy persists at 12
Consultations
- Call toxicologist on call (Poisons Information Centre 13 11 26)
- If any signs of envenomation are present.
- For all potential snakebites in paediatric patients.
- If the patient was bitten by a snake in a location other than Victoria or Tasmania.
- If the patient is a snake handler or the bite was from an exotic snake.
- If there is any doubt about treatment.
Discharge Criteria
- Normal neurological
- Normal blood parameters
- Vomiting
- Tolerating diet and
- Ambulating
- Do not discharge
Hospital admission criteria
- Respiratory distress requiring ventilatory
- VICC resulting in clinically significant
- Post cardiac arrest / circulatory
Definition
- Neurological dysfunction caused by focal brain or retinal ischaemia lasting <1hr
- Typical duration 2-15min
Admission Criteria
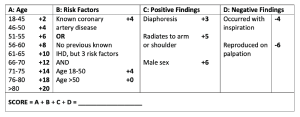
Rothwell ABCD2 score
- Components
- Age >60 =1 point
- BP> 140/90 = 1 point
- Clinical features
- Unilateral weakness = 2 points
- Speech impairment without weakness= 1 point
- Duration of symptoms
- >60min = 2 points
- 10-59 min= 1 point
- Diabetes= 1 point
- Scoring
- >5= high risk
- 7 day stroke risk 25-30%
- Admit medical
- 4-5= moderate risk
- 7 day stroke risk 20-25%
- For SSOU to complete investigations as inpatient
- Score 0-3=-3 low risk
- 7 day stroke risk 0-15%
- Safe for home or SSOU. Investigations can be completed as outpatient
- >5= high risk
Exclusion criteria
If present refer to medical team for admission
- Score ≥ 6
- Unstable vital signs
- New AF
- History of recent head trauma
- Abnormal new CT scan findings
- Neurological signs not resolved
- Crescendo TIAs (ie >1 TIA)
Investigations
- CTB +/- angiography +/- stroke protocol
- ECG
- FBE
- UEC
- Fasting lipids
- BSL
- HbA1c if diabetic
- Additional as required
- Carotid Doppler- for anterior circulation
- TTE if AF
- MRI in selected patients
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Antiplatelet |
|||
|
Aspirin |
300mg if loading required then 100mg daily |
Daily |
PO |
|
OR Clopidogrel (if already on aspirin) |
75mg |
Daily |
PO |
|
Antihypertensives
|
|
|
|
|
Consider ACE inhibitor |
|||
|
Lipid lowering agent |
|||
|
Atorvastatin |
80mg |
Daily |
PO |
|
Or increase current to max dose |
|
|
|
Specific observations
- Telemetry
Report immediately to medical staff any of the following
- Notify if any irregularity in pulse rhythm e.g. new AF
Discharge Criteria
- Responsible carer to observe
- Follow-up arrangements made
- Adequate explanation and understanding
- Education regarding stroke risk, risk factor management and signs and symptoms of stroke
- Stopping smoking- 66% relative risk reduction from cessation
- Low fat and salt diet
- Increasing regular exercise
- Avoiding excessive ETOH- no more than 2 STD per day
- Advice re driving
- Appropriate medications changes with script
Hospital admission criteria
- Neurological deficit persists
- Evolving causative pathology- consider transfer
- Abnormal CT or critical Doppler abnormality
- >80% stenosis risk decreased by 50% with endarterectomy/ stenting and 25% for 70-80% stenosis
- Patients with lesser stenosis do not benefit from surgery
- Unable to establish safe discharge environment
Follow-up
- Medical TIA clinic as OP
Definition
- Urinary retention is the acute or chronic inability to voluntarily pass an adequate amount of urine. The condition predominantly affects men. The most common causes are obstructive in nature, with benign prostatic hyperplasia accounting for 53% of cases.
- Causes
- BPH/ prostatitis
- Urethral strictures- post trauma, infection, radiation, surgery, clot retention
- Prostate cancer/ penis cancer
- Phimosis/ paraphimosis
- Acute prostatitis/ urethrities
- Pharmacology
- Anticholinergics
- Sympathomimetics
- CCB
- TCA
- Antihistamines
- Neurogenic causes
- MS
- Parkinsons
- Diabetic perihperal neuropathy
- Spinal trauma
- Strokes
- Infection/ inflammatory
- Genital herpes
- Constipation
Admission Criteria
- Male patient
- Retention of urine
- Catheterized via the urethra
- Physical obstruction
- Afebrile
- Normal lower limb neurology
Exclusion criteria
- Failed urethral catheterization
- Significant co-morbidities
- Patient unlikely to cope with leg bag/ management at home
- Trauma
- Neurological cause for obstruction
- Post urological surgery e.g. clot retention
Investigations
- FBE
- UEC
- Urine FWT / MCS
- Bladder scan prior to IDC insertion
- +/- CTAP
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Alpha blockers e.g. Tamsulosin |
AFTER DISCUSSION WITH UROLOGIST |
||
|
Apperients if due to constipation |
|
|
|
|
Paracetamol |
1g |
4hrly PRN max 4g |
PO |
|
Normal saline |
1000ml- to match urine output if post obstructive diuresis |
As required |
IV |
Specific observations
- Urine output >200ml/hr following drainage
- Requires referral to urology for post obstructive diuresis
- Haematuria- except from initial insertion if traumatic
- Report increasing abdominal discomfort
- Report fever
Consultations
- Discussion with urology
Discharge Criteria
- Catheter education
- Referral to district nursing if required
- Clear follow-up plan with patient aware of plan
Hospital admission criteria
- Development of fever
- Development of haematuria
- Systemic toxicity
Follow-up
- Trial of void clinic
Definition
- Illusion of motion, rotatory or otherwise
- Important to distinguish peripheral vertigo (caused by lesions of the vestibular nerve and inner ear) from central vertigo (caused by lesions of the CNS)
- Peripheral vertigo
- approximately 90% of cases
- may be very sudden onset when due to benign positional vertigo
- nystagmus usually present
- horizontal or horizontal-rotatory
- not vertical, unless following Dix-Hallpike test
- unidirectional
- never direction changing
- initially toward affected ear
- horizontal or horizontal-rotatory
- Causes
- Meniere’s disease
- labyrinthitis
- benign paroxysmal postural vertigo (BPPV)
- acoustic neuroma
- Central vertigo
- approximately 10% of cases
- may be sudden in onset when caused by stroke
- usually slow in onset when due to other causes (tumour, demyelination etc)
- is usually less severe and causes less nausea and vomiting than peripheral causes
- nystagmus
- usually absent
- vertical nystagmus may occur without vertigo
Admission Criteria
- Acute vertigo with peripheral aetiology as per HINTS exam
Exclusion criteria
- Severe headache
- Significant ataxia e.g. cannot walk
- Recurrent or worsening vertigo
- Fever
- Cranial nerve abnormalities
- Cerebella dysfunction
- ANE long tract neurological signs
- Examination findings suggestive of central cause - indication for medical admission.
Investigations
- FBE
- UEC
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Paracetamol |
1g |
4hrly PRN max 4g |
PO |
|
Prochlorperazine |
12.5mg |
6hrly |
IV/ IM |
|
Prochlorperazine |
10mg |
6hrly |
PO |
|
Nasline |
1000ml |
Maintain hydration |
IV |
|
Consider Eply maneuver |
|||
Specific observations
- Monitor for altercation in conscious state
Specific management issues
- Bed rest and supervised mobilization until physio review
- Report any of
- Worsening vomiting or vertigo
- Altered conscious state- GCS falling by 1 point or more
- Severe headache
- Facial or motor asymmetry
- IVF until tolerating oral
Consultations
- Medical if symptoms persist or new neurological changes develop
- Physiotherapy if required
Discharge Criteria
- Symptoms resolved, passed mobility test
- Appropriate carer
- Follow-up arranged
- Consider discharge medication
Hospital admission criteria
- Persisting symptoms
- Dehydration not resolved
- Development of new neurological symptoms
Definition
- High INR awaiting normalization to safe therapeutic level
Admission Criteria
- INR >5.0 on warfarin therapy
- Minor bleeding only and controlled in ED
- Drug interaction considered/ eliminated
- Systolic BP <180mmHg
Exclusion criteria
- Uncontrolled bleeding any site
- Falls risk
- Significant bleeding, non compressible e.g. GIT, intracerebral, haemoptysis
Risk factors for bleeding- 2 or more suggest HIGH risk
- Age > 65yrs
- Uncontrolled hypertension
- History of GI haemorrhage, active peptic ulcer, hepatic insuffi ciency
- Haematogical: platelet count < 50 109/L OR dysfunction, coagulation defect, malignancy
- History of stroke, cognitive or psychological impairment
- Renal insuffi ciency
- Trauma: recent trauma, > 3 falls within previous treatment year, recurrent or injurious falls
- Excessive alcohol intake
- Medications: Asprin, NSAIDs, COX-II, “ natural remedies”
Investigations
- INR
- FBE
- UEC
- LFT
- Additional as required
- Repeat INR 6hrs and 12hrs after initial treatment if not normalized
Suggested medications
|
INR |
Bleeding risk YES/ NO |
Risk of bleed |
Reversal agent |
|
5-9 |
No |
Low |
Consider 1mg vitamin K |
|
5-9 |
No |
High |
Vit K 1-2mg orally OR 0.5-1mg IV |
|
>9 |
No |
Low |
Vit K 2.5-5.0mg PO OR 1mg IV |
|
>9 |
No |
High |
Vit K 1mg IV OR Prothrombinex 25-50 units OR FFP 150-300mls IV |
Specific observations
- Any new bleeding/ malena
Specific management issues
- Stop warfarin for 24hrs and restart next night at ½ usual dose
Discharge Criteria
- INR < 5 and no bleeding
- Repeat INR in 24 hours after discharge
- Any drug interaction resolved
- Patient understands cause of toxicity
- Review need for ongoing warfarin
- Restart WARFARIN AFTER 24 HOURS at ½ dose
Hospital admission criteria
- Development of significant haemorrhage
- INR > 5
- Failure to control minor haemorrhage or recurrence
Definition
- Intentional or non-intension potential dangerous ingestion of paracetamol
- Risk assessment
- Dose
- Formulation ingested
- Acute vs staggered vs repeated supratherapeutic
- Time of ingestion
- Symptoms- abdo pain, N/V
- Clinical features
- Usually asymptomatic
- Abdominal pain, vomiting
- Late toxicity- liver failure, coagulopathy, encephalopathy
- Refer to Austin Toxicology clinical practice guidelines and call Poisons Information Centre as required on 13 11 26 for clinical advice
Admission Criteria:
- Overdose paracetamol
- Cleared ECAT or likely DC home rather than Psychiatry admission
- 4hour ED observation or a clear period in which physiological stability is assessed and documented
Exclusion criteria
- Known ingestion of potentially lethal material
- Patient on Assessment Order
- Abnormal neurological examination inc seizures, hallucinations, confusion, or GCS 14-15
- Unstable respiratory or cardiovascular status
- Abnormal LFTs/ Coagulation profile
- Cardiac arrhythmias
- Need for ongoing decontamination procedures
- Ingestion of corrosives
- Ongoing suicidal intent and uncooperative with treatment
Investigations
- 1st paracetamol level (4hrs from ingestion)
- LFTs
- Blood Alcohol level
- ECG
- Additional as required
- FBE
- INR / coagulation
- BSL
- Repeat bloods
Paracetamol nomogram
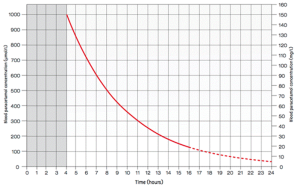
Management
- 4hrs post ingestion- Paracetamol level and LFTs
- Plot paracetamol level on nomogram and if above treatment line treat with 20hour NAC course
- 2 hours prior to completion of 20-hour NAC course
- Measure ALT
- Paracetamol level
- If ALT is abnormal or paracetamol level onc >10mg/L continue NAC and refer to medical team for admission
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Metoclopramide |
10mg |
8hrly PRN |
IV/ PO |
|
Ondansetron |
8mg |
8hrly PRN |
SL/ IV |
|
Pink mix |
10ml/20ml |
PRN |
PO
|
|
Loratadine |
10-20mg |
Once PRN |
PO |
|
NAC (Acetylcysteine) ADULT |
|||
|
1st dose: |
200mg/kg in 500ml 5% glucose |
Over 4hrs |
IV |
|
2nd dose: |
100mg/ kg in 1000ml 5% glucose |
Over 16hrs |
IV |
Specific observations
- Report evidence of allergic reaction to NAC (rash, itch, orofacial swelling, dyspnoea)
Consultations
- ECATT
Discharge Criteria
- Return of non toxic/ normal laboratory results
- Stable vital signs/ neurological exam
- ECATT assessment completed and deemed safe for discharge
- Safe psychosocial environment with appropriate care
Hospital admission criteria
- Abnormal laboratory results
- Deterioration in neurological state or GCS
- Cardiac/ respiratory instability
- Unsafe psychosocial environment
- Persistent suicidal intent
Discharge follow-up
- Mental health team
- GP
Definition
- Mild head trauma related to transient neurological or systemic dysfunction
Admission Criteria
- GCS 14-15
- Age 16-65
- Mild head injury without dangerous mechanism, requiring period of observation (4-6hours)
- LOC <5min
- Isolated injury
- Normal CTB (Canadian Head CT rules for indications)
- Mild headache
- Mild nausea/ single vomit
- No cpsine collar
Canadian Head CT rule (Indications for head CT in minor head injury)
- High risk (for neurological intervention)
- GCS score <15 at 2 h after injury
- Suspected open or depressed skull fracture
- Any sign of basal skull fracture (haemotympanum, ‘racoon’ eyes, cerebrospinal fluid otorrhoea/rhinorrhoea, Battle’s sign)
- Vomiting ≥ two episodes
- Age ≥ 65 years
- Medium risk (for brain injury on CT)
- Amnesia before impact >30 min
- Dangerous mechanism (pedestrian struck by motor vehicle, occupant ejected from motor vehicle, fall from height >3 feet or five stairs)
Exclusion criteria
- Abnormal CT
- Repeated/persistent Vomiting
- Focal neurological sign
- Skull fracture
- Facial fractures
- LOC > 5 minutes
- Deterioration in GCS> 1 point
- Pre injury debility or non ambulant
- Risk of cervical spine injury / collared
- Age > 65
- Intoxicated / Drug affected
Investigations
- CTB as per NUTS Head Injury Guidelines
- CTB if coagulopathy present inc NOAC, clopidogrel
- BSL
- BAL

Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Paracetamol |
1g |
4hrly PRN max dose 4g 24hrs |
PO |
|
Ibuprofen |
400mg |
6hrly PRN |
PO |
|
Oxycodone IR |
5-10mg |
4hrly PRN |
PO |
|
Metoclopramide |
10mg |
8hrly PRN |
PO/ IV |
|
Ondansetron |
8mg |
8hrly PRN |
SL/ IV |
Specific observations
- Abbreviated Westmead Post traumatic amnesia scale if any amnesia
- Report persistent vomiting, increasing headache, falling GCS, developing neurology
Consultations
- Neurosurgery or surgical if symptoms not improving or deteriorating
Discharge Criteria
- Normal neurological exam at discharge with GCS 15
- Clinically improving
- Passed A-WPTAS if required
- Normal CTB or NO indication for CTB
- Appropriate carer and able to return if condition deteriorates
- Able to take & tolerate oral fluids
- Head injury information supplied and understood
Hospital admission criteria
- Development of exclusion criteria
- Persisting abnormal mental state
- Uncontrolled headache, vomiting
- Lack of appropriate carer
Definition
- A peritonsillar abscess (also called paratonsillar abscess or quinsy) is a collection of pus in the space between the tonsil and the superior pharyngeal constrictor muscle.
- Tonsillitis is inflammation and infection of the tonsils
Admission Criteria
- Severe pharyngotonsilitis
- Systemic toxicity
- Dysphagia, unilateral sore throat
- Dehydration
- Difficulty opening mouth (trismus)
Exclusion criteria
- Airway compromise
- Stridor
- Uncertain site
- Abscess needing intra-operative drainage
- Immune-compromise
Investigations
- FBE
- UEC
- Additional as required
- EBV screen- monospot/ serology
- Throat MCS
- Consider need for aspiration/ formal I&D
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
0.9% Nasline |
1000ml |
4-12hrly |
IV |
|
Benzylpenicillin |
1.2g |
6hrly |
IV |
|
Dexamethasone |
8mg |
12-24hrly |
IV |
|
Paracetamol |
1g |
4hrly PRN max dose 4g |
PO or IV |
|
Ibuprofen |
400mg |
6hrly |
PO |
|
Aspalgan (aspirin/ codeine) gargle |
900/30mg |
BD |
Gargle |
|
Lignocaine viscous |
10-20ml |
TDS prior to meals |
PO |
Specific observations
- Report stridor or worsening dysphagia to medical staff
- Pain score hourly and give analgesia until pain adequately controlled
Specific management issues
- If abscess aspirated diet as tolerated
Discharge Criteria
- Adequate hydration/ tolerating oral fluids
- Normal vital signs
- Pain controlled
Hospital admission criteria (TF to Melbourne as no ENT service at Bendigo)
- Inadequate hydration or ability to tolerate oral fluids
- Persisting toxicity
- Requiring formal I&D of abscess
Definition
- Nausea and vomiting is the most common medical condition in pregnancy, affecting up to 90% of women.
- Persistent vomiting that leads to weight loss of greater than 5% of pre-pregnancy weight occurs in 1% of pregnancies and is referred to as hyperemesis gravidarum. This is associated with electrolyte abnormalities and dehydration
Admission Criteria
- Presumed normal pregnancy
- Vomiting requiring IV hydration
- No evidence of miscarriage
- No evidence of pre-eclampsia
- Other diagnosis unlikely (e.g. UTI, surgical abdomen)
- Normal urinalysis
Exclusion criteria
- Diagnosis unclear
- Abdominal pain/ tenderness unrelated to vomiting
- Urinary symptoms
- PV bleeding
- Fever
- >20 weeks gestation
- BP >140/90 and proteinuria or symptoms of possible pre-eclampsia (seizure, headache, blurred vision, abdominal pain)
Investigations
- FBE
- UEC
- Glucose
- CMP
- LFT
- Urine FWT
- Consider
- USS if pregnancy not yet sited
- BHCG is NOT indicated unless pregnancy has not been sited- as grossly elevated levels may suggest molar pregnancy
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Pyridoxine |
25mg |
TDS |
PO |
|
Doxylamine (restavit) |
12.5-25mg |
Nocte (TDS if tolerated) |
PO |
|
Metoclopramide |
10mg |
TDS |
IV/ PO |
|
Prochlorperazine |
5-10mg 12.5mg |
TDS TDS |
PO IV |
|
Ondasnetron |
4-8mg |
TDS |
SL/ IV |
|
Hartmann’s (CSL) |
1000ml |
2-8hrly PRN |
IV |
Consider review RWH guidelines for ‘Nausea and vomiting- Pregnancy’
Specific observations
- Report any
- PV bleeding
- Increasing abdominal pain and or vomiting
- Increased BP
- Altered conscious state, headache, blurred vision
Specific management issues
- Bland diet
- Consider laxatives if constipation also present
Consultations
- Gynaecology
Discharge Criteria
- Nil vomiting for 6 hours
- Normal hydration
- Able to tolerate fluids
- Adequate social support and carer
- Follow-up arranged
- Script for regular/ PRN antiemetics
- RWH Patient handout for ‘Coping with Nausea and vomiting in Pregnancy’
Hospital admission criteria
- Vomiting persisting
- Unable to tolerate oral fluids and antiemetics
- PV bleeding or increasing abdominal pain
Discharge Follow-up
- GP
- Private obstetrician
Bendigo ED/SSOU Cellulitis Guideline
PURPOSE AND SCOPE
To assist ED and SSOU staff in the diagnosis and management of cellulitis
To reduce the length of ED/SSOU stay of patients with cellulitis, and to reduce the rates of unsuccessful SSOU admissions
To assist in making early and appropriate disposition decisions
KEY POINTS
|
Consider key differential diagnoses Most uncomplicated cases of cellulitis do not require investigation Oral antibiotics are suitable for most patients. Intravenous antibiotics should only be used for those with evidence of severe infection, uncontrolled comorbidities, failure of oral antibiotics or specific circumstances that may limit oral therapy Spreading erythema, ongoing fever and lymphangitis <72 hours after commencing appropriate antibiotics does not necessarily constitute failure of oral therapy. Consider a longer course or higher dose of oral antibiotics Rest, elevation and splinting/immobilisation of any affected limb in order to reduce lymphatic spread are just as important as antibiotics in the successful treatment of cellulitis Under certain circumstances, patients may need investigation and management by units other than ED/SSOU |
OVERVIEW
Cellulitis is a spreading bacterial infection of the skin. There may be associated lymphangitis, lymphadenopathy, fever or haemodynamic compromise.
Impetigo is a highly contagious infection of the epidermis, particularly common in young children (hence known as “school sores”), often notable for its characteristic honey-coloured crust.
Common aetiology:
- Streptococcus spp or Staphylococcus aureus
- Purulent cellulitis is caused by Staphylococcus aureus
- Cellulitis associated with animal bites (Capnocytophagia, Pasteurella, Eikenella), fresh water exposure (Aeromonas spp) or salt water exposure (Vibrio spp) require specific antibiotic regimes – refer to eTG for the most up to date recommendations
- Cellulitis caused by MRSA is uncommon but is associated with penetrating trauma or ulcerated wounds
- In immunocompromised patients, there are many possible causes which may include Gram negative bacteria, fungi or mycobacteria
Many conditions can present similarly to cellulitis, and are therefore often not treated appropriately. Consider the following differential diagnoses:
- Necrotising fasciitis is a rare but life-threatening infection causing necrosis of subcutaneous tissues and fulminant sepsis. It can be caused by Group A streptococcal species, Clostridium species spp, or be polymicrobial. It presents as rapidly spreading erythema, severe pain +/- gas in tissues (crepitus) and haemodynamic compromise, mostly in diabetic and immunosuppressed patients. It requires urgent IV antibiotics and source control through surgical debridement by the Plastics team. Fournier’s gangrene is an acute necrotising infection of the perineum or genitalia and should be referred urgently to Urology
- Lipodermatosclerosis is a chronic, often bilateral inflammatory condition of the lower limb associated with venous insufficiency causing oedematous brown-red discolouration of the skin. It does NOT respond to antibiotics. Bilateral lower limb cellulitis is rare and more likely to be lipodermatosclerosis
- Varicose eczema
- Joint pathology: septic arthritis, gout/pseudogout, inflammatory arthritis
- DVT
- Hypersensitivity reaction
- Pyoderma gangrenosum
Predisposing factors to cellulitis include any skin breech, IV drug use, lymphoedema, chronic venous insufficiency, peripheral vascular disease, diabetes, obesity, tinea, fissured dermatitis and CCF.
Local audits and published studies have shown that patients with cellulitis have relatively long admissions to SSOU, high rates of unnecessary SSOU admission, and high rates of unsuccessful SSOU admissions. These factors demonstrate a need to identify the likely trajectory of the patient’s illness, and to admit/refer appropriately and early. The rates of necessary admission with cellulitis have been estimated at less than 10%, however this rate increases significantly in patients 55 years or older.
CLINICAL PRESENTATION
Acute onset of skin erythema, warmth, tenderness and swelling +/- lymphangitis, lymphadenopathy or systemic features.
Severe cellulitis is defined by the presence of cellulitis AND hypotension, or cellulitis plus two or more of the following:
- Temperature >38.0 or <36.0
- HR >90
- RR >20
- WCC <4 or >12 (or >10% bands)
- Risk factors: IV drug use, immunocompromise, diabetes
Violaceous colour or the presence of bullae are highly suggestive of severe or systemic infection by organisms such as Vibrio or Streptococcus pneumoniae, and should be treated as such.
Pain out of proportion to clinical findings, palpable crepitus, hypotension and rapid spread of cellulitis should raise concern for a necrotising infection and an urgent surgical consult should be sought.
INVESTIGATIONS
Most uncomplicated cases of cellulitis DO NOT require investigation.
FBE, UEC, LFTs, CRP and blood cultures are only required if the patient is systemically unwell, is immunosuppressed, has significant comorbidities (including valvular heart disease, prosthetic heart valve) or where liver/renal dysfunction may affect the dose or choice of antimicrobials.
Blood cultures should not be routine; only in patients with sepsis or where atypical organisms are suspected.
US should be utilised if a foreign body is suspected, and to identify and quantify abscesses for surgical drainage.
MANAGEMENT
Patients are commonly referred to hospital for IV antibiotics after “failure of oral therapy”.
Rest, elevation and splinting/immobilisation of any affected limb in order to reduce lymphatic spread are just as important as antibiotics in the successful treatment of cellulitis.
Non-adhesive dressings should be applied to eroded skin.
Do NOT draw around the edge of cellulitis (see note below*).
Incision and drainage is the definitive treatment for abscesses – only patients with signs of systemic infection, or cellulitis extending beyond the abscess require antibiotic therapy.
Oral antibiotics are suitable for most patients.
Intravenous antibiotics should only be used for those with evidence of sepsis, uncontrolled comorbidities, failure of oral antibiotics (see note below*), or under specific circumstances (see section “Inpatient Management”)
* Spreading erythema, ongoing fever and lymphangitis <72 hours after commencing appropriate antibiotics does not necessarily constitute failure of oral therapy. Erythema often progresses after treatment is initiated and bacterial toxins are released. If otherwise clinically improving and no evidence of sepsis, oral antibiotics should generally be continued, and the need for rest/elevation/immobilisation reiterated. Consider increasing the dose of oral antibiotics (see outpatient management below).
Cellulitis associated with bites (either human or animal) should be referred to AGSU for consideration of washout +/- surgical debridement under general anaesthesia.
OUTPATIENT MANAGEMENT
Rest, elevation and splinting/immobilisation if a limb is affected is imperative to treatment.
Consider a tetanus booster (if not up to date) if cuts, bites or abrasions are suspected to be the cause of cellulitis.
Impetigo can be treated with topical mupirocin ointment, or cephalexin if widespread or large lesions.
|
1. Mupirocin ointment 2% to affected areas TDS for 5 days OR 2. Cephalexin 33mg/kg (max 500mg) PO BD for 5 days |
Oral flucloxacillin is considered first-line treatment for adults with cellulitis due to its narrow spectrum of activity against Staphylococcal and Streptococcal species. Cephalexin has broader activity against Gram negative organisms, which can alter intestinal flora and lead to antibiotic resistance in these organisms. There is emerging resistance against erythromycin and roxithromycin in Staphylococcus and Streptococcus species. Cephalexin is preferred for use in children with mild cellulitis due to the poor palatability of flucloxacillin. Note the reduced frequency of dosing in children.
|
1. Flucloxacillin 500mg PO QID for 5 days OR 2. Cephalexin 500mg PO QID (paediatrics: 33mg/kg (max 500mg) TDS) for 5 days |
Clindamycin is the antibiotic of choice for patients with severe hypersensitivity to penicillins or cephalosporins. Be mindful though that there is an increased risk of antibiotic-associated diarrhoea and Clostridium difficile colitis. Note the increased frequency of dosing in children.
|
1. Clindamycin 450mg PO TDS (paediatrics: 10mg/kg (max 450mg) QID) for 5 days |
MRSA is an uncommon cause of cellulitis but may be associated with penetrating or ulcerated wounds. Risk factors include:
- Residence in an area with a high prevalence of MRSA (NT, remote communities in northern Queensland, some areas of WA)
- Patients of ATSI or Pacific Island descent
- Previous colonisation or infection with MRSA
- Frequent hospital stays, especially if associated with surgery
- Residence in an aged-care facility, especially if the patient has had multiple courses of antibiotics
For proven or suspected MRSA infections, use clindamycin or trimethoprim/sulfamethoxazole.
|
1. Clindamycin 450mg PO TDS (paediatrics: 10mg/kg (max 450mg) QID) for 5 days OR 2. Trimethoprim/sulfamethoxazole 160/800mg (paediatrics 8/40mg (max 320/1600mg)) PO BD for 5 days |
Patients with persistent skin changes after 5 days of oral therapy, but who are otherwise systemically well, should be considered for a longer course of oral antibiotics (10-14 days in total), or a higher dose of oral antibiotics (e.g. flucloxacillin 1000mg QID for 5 days OR cephalexin 1000mg QID for 5 days).
It should be noted, however, that prolonged or high dose treatment with flucloxacillin has been associated with rare cases of severe cholestatic hepatitis. The incidence of this reaction has been estimated to be between 1 in 12,000 and 1 in 100,000. The risk is predominantly in patients who are greater than 55 years of age, or who are treated for more than 14 days. Consider the patient’s individual circumstances, changing to another agent if longer or high dose therapy is required (e.g. cephalexin), and careful monitoring of liver function during treatment.
INPATIENT MANAGEMENT
This can occur in SSU (if anticipated stay is <24 hours), HITH, AMU or other inpatient specialty units depending on location, comorbidities and likely duration of treatment. Paediatric patients not requiring surgical input should be referred to the Paediatrics team.
Patients requiring hospital admission for IV antibiotics:
- Sepsis or significant comorbidities (IV drug use, immunosuppressed, chronic heart/lung/liver/renal disease, diabetes) – SSOU or AMU
- Not tolerant of oral intake
- Genuine failure of oral antibiotics
- Suspected necrotising infections – urgent AGSU (Plastics) referral (or Urology in cases of Fournier’s gangrene) plus IV antibiotics as per eTG and allergy history
- Diabetic foot ulcer with associated cellulitis – AMU, may need discussion with a Vascular service
- Cellulitis complicating penetrating injuries and retention of foreign bodies – AGSU (Plastics)
- Hand cellulitis – consider AGSU (Plastics) referral
- Cellulitis of finger/hand with concern for tenosynovitis – AGSU (Plastics)
- Orbital cellulitis – transfer to a Melbourne-based service with an ENT/Ophthalmology service
- Cellulitis associated with an abscess that requires inpatient incision and drainage (AGSU (Plastics))
- Cellulitis associated with either animal or human bites – AGSU (Plastics) for consideration of washout under general anaesthesia
- Social issues that will significantly impact upon care – SSU or AMU
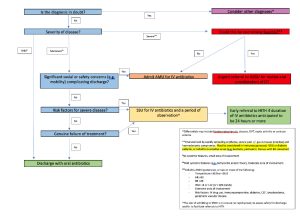
Figure 1: Disposition for patients with cellulitis
When systemic features have resolved, switch to oral therapy – this may occur as rapidly as 1 or 2 doses of IV antiobiotics. A total of 5-10 days duration of treatment is recommended.
Antibiotic choice:
|
1. Flucloxacillin 1-2g (paediatrics: 50mg/kg (max 2g)) IV QID OR 2. Cephazolin 1-2g IV TDS |
Clindamycin can be used in patients with severe cellulitis who have either an immediate or severe allergy to penicillins/cephalosporins, or if MRSA infection is suspected or proven and the organism is considered susceptible (based on sensitivity testing and local strain susceptibility)
|
1. Clindamycin 600mg (paediatrics: 10mg/kg (max 600mg)) IV TDS |
For proven or suspected MRSA infections, use vancomycin or clindamycin (depending on sensitivities if proven to be the cause of infection)
|
1. Vancomycin IV (refer to eTG, AMH Handbook and RCH website for dosage and principles of use) OR 2. Clindamycin 600mg (paediatrics: 10mg/kg (max 600mg)) IV TDS |
If community-based IV treatment is appropriate, please discuss with the Hospital In The Home (HITH) team as soon as possible. Patients typically suitable for their service have risk factors for severe disease, extensive areas of cellulitis or are not responding to appropriate oral antibiotics. They must meet the following criteria:
- resolution of systemic features
- no associated abscess (may require US to exclude)
- no concern for limb compromise
- exclusion of other diagnoses (where appropriate) prior to acceptance of care (e.g. DVT or abscess)
- must live within a 30km radius of Bendigo, or be able to reside somewhere within this radius (e.g. with a relative or friend); patients outside of this area may be accepted for brokerage following review and in consultation with HITH nursing staff
- must have access to a phone and carer in the event of an emergency
- patient or appropriate medical decision maker must provide consent to treatment
- patient and their home environment (e.g. pets) must not pose a threat to the safety of staff
The antibiotic of choice for HITH patients with cellulitis is cephazolin (due to its less frequent dosing), with or without probenecid (see below).
|
1. Cephazolin 2g IV daily PLUS Probenecid 1g PO daily OR 2. Cephazolin 2g (paediatrics 50mg/kg (max 2g)) IV BD |
Probenecid is a medication that increases the excretion of uric acid into the urine. It is typically used in the treatment of gout and hyperuricaemia. Studies have also shown that probenecid increases the serum concentration of penicillins and cephalosporins by inhibiting their renal excretion, making once or twice daily dosing possible in the community via HITH.
It is not used in paediatric patients with cellulitis.
It should not be used when gout is active and can sometimes precipitate liver dysfunction and uric acid kidney stones so should be used cautiously in these instances.
OTHER
Fungal infection of the toes and their interspaces can provide a portal of entry for bacterial invasion – patients with lower extremity cellulitis (particularly if recurrent) may require antifungal therapy in addition to antibiotics
Patients with cellulitis associated with chronic wounds and other chronic conditions (such as lymphoedema, diabetes or peripheral vascular disease) may benefit from referral to a number of available community-based services:
- High risk foot clinic
- Lymphoedema service
- Wound clinic
- RDNS (now known as Bolton Clarke)
REFERENCES
Electronic Therapeutic Guidelines (eTG) - Cellulitis and erysipelas [Internet]. Melbourne, Australia: Therapeutic Guidelines Ltd; April 2019 [amended August 2021, accessed January 2021]. Available from https://tgldcdp.tg.org.au.acs.hcn.com.au/viewTopic?topicfile=cellulitis-erysipelas&guidelineName=Antibiotic&topicNavigation=navigateTopic#MPS_d1e491
Abetz JW, Adams NG, Newnham H, Smit V, Mitra B. Transfer of care and overstay in the management of cellulitis in the emergency short stay unit: A retrospective cohort study. Emerg Med Australas. 2017 Apr;29(2):143-148. doi: 10.1111/1742-6723.12731. Epub 2017 Jan 22. PMID: 28111931.
Cox VC, Zed PJ. Once-daily cefazolin and probenecid for skin and soft tissue infections. Ann Pharmacother. 2004 Mar;38(3):458-63. doi: 10.1345/aph.1D251. Epub 2004 Jan 23. PMID: 14970368.
Long B, Gottlieb M. Diagnosis and Management of Cellulitis and Abscess in the Emergency Department Setting: An Evidence-Based Review. J Emerg Med. 2022 Jan;62(1):16-27. doi: 10.1016/j.jemermed.2021.09.015. Epub 2021 Oct 14. PMID: 34657784.
Clinical Practice Guidelines: Cellulitis and other bacterial skin infections [Internet]. Melbourne, Australia: Royal Children’s Hospital; March 2020 [accessed February 2022]. Available from https://www.rch.org.au/clinicalguide/guideline_index/Cellulitis_and_skin_infections/
Hospital In the Home (HITH) Admission and Referral Protocol [Bendigo Health Intranet]. Bendigo, Australia: Bendigo Health; 2017 [accessed February 2022]. Available from https://app.prompt.org.au/search
|
Original Author: Dr Scott Taylor Publication Date: July 2022 Amendment Date: January 2023 Review Date: July 2025 |
Definition
- Chest pain can be caused by a number of different pathologies which may include
- Ischaemic chest pain
- Pulmonary embolism
- Pneumonia
- Pneumothorax
- Gastritis
- Pericarditis
- Aortic dissection
- Among many others
- Ischaemic chest pain may be stable angina, unstable angina, NSTEMI and STEMI
Admission Criteria
- Pain/ other symptoms resolved
- Risk stratification intermediate or low requiring investigations
- Serious non cardiac cause clinically unlikely
- Stable rhythm
- Stable vital signs
- No acute ischaemic ECG changes
- 1st troponin expected to be in normal range in low risk patients
Exclusion criteria
- Persistent symptoms e.g. pain, dizziness, dyspnoea
- Unstable or abnormal vital signs
- Risk stratification high
- Unstable cardiac rhythm
- Abnormal ECG
- Cardiac enzyme rise
Scoring system
EDACS Emergency Department Assessment of Chest pain score
- Calculate EDACS score via MDCALC
- Chest pain present for >6hrs = single troponin
- EDACS <16 repeat troponin 2hrs
- EDACS >=16 repat troponin 3hrs
Investigations
- FBE
- UEC
- Troponin
- 12 lead ECG
- Consider
- CXR- this may not always be required, consider when patient has last had a CXR and if this is clinically indicated
- D-dimer- if requesting this please refer to “Pulmonary Embolism Pathway”
- Additional
- Requested repeat troponin with appropriate time to be taken
- Repeat 12 lead ECG with second troponin
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Aspirin |
300mg |
Once |
PO |
|
GTN |
300-600mcg |
PRN 5min |
SL |
|
Paracetamol |
1g |
PRN 4hrly |
PO |
|
Oxycodone IR |
5-10mg |
PRN 4hrly |
PO |
|
Ondansetron |
4-8mg |
PRN 8hrly |
SL/ PO |
|
Metoclopramide |
10mg |
PRN 8hrly |
PO |
Specific observations
- Cardiac monitoring
- Report any chest/ arm/ jaw discomfort or shortness of breath to SSOU HMO. Please complete a repeat ECG.
- Repeat ECG to be reviewed by senior SSOU doctor
Consultations
- Consider discussion with cardiology
Discharge criteria
- Resolved pain, no further symptoms
- Unchanged ECG
- No troponin rise
- Follow-up arranged
Admit to hospital if any of the following apply
- Recurrent chest pain or significant symptoms
- ECG changes/ arrythmia
- Troponin rise
Discharge follow-up
- Follow-up testing is not required if patient is <50yo AND has <3 risk factors AND no previous CAD or MI
Definition
- A pulmonary embolism (PE) is a blood clot that develops in a blood vessel elsewhere in the body (often the leg) and travels to an artery in the lung, causing a sudden blockage of blood flow to part of the lungs
- Annual incidence of 0.31 per 1000 in Australia
Admission Criteria
- Stable vital signs
- No O2 requirement
- No increased WOB
- ECG- no signs of right heart strain
- Low or Very Low Risk PESI score
- PERC score >0 (as if 0 will rule out PE)
Exclusion criteria
- PERC 0
- PESI score risk class 3-5
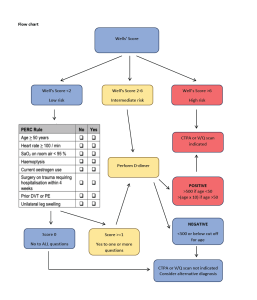
Scoring system
- Calculate Wells score to determine need for d-dimer and CTPA
- If patient low risk calculate PERC score
- If PERC 0 <2% chance of PE indicating no need for further work-up for PE
- If PERC >=1 D-dimer is required
- If patient Intermediate or high risk consider CTPA or VQ scan
- If patient low risk calculate PERC score
- Calculate PESI score to determine mortality risk if patient has PE
- If Very Low Risk or Low Risk PE – can go to SSOU
- If risk class 3-5 requires medical admission
PERC Score
|
Criteria |
Point |
|
Age >= 50 years |
1 |
|
Heart rate >= 100bpm |
1 |
|
SaO2 on room air <95% |
1 |
|
Haemoptysis |
1 |
|
Current oestrogen use |
1 |
|
Surgery or trauma requiring hospitalization within 4 weeks |
1 |
|
Prior DVT or PE |
1 |
|
Unilateral leg swelling |
1 |
Score
- 0 points or No to all = <2% risk of PE
- >=1 or yes to any= cannot rule out PE
WELLS Score
|
Criteria |
Points |
|
Clinical signs/ symptoms of DVT |
3 |
|
PE most likely diagnosis |
3 |
|
Tachycardia (>100bpm) |
1.5 |
|
Immobilisation/ surgery in previous 4 weeks |
1.5 |
|
Prior DVT/ PE |
1.5 |
|
Haemoptysis |
1 |
|
Active malignancy (treatment within last 6months) |
1 |
Score
- Low risk <2 points- 2-4% probability of PE
- Intermediate risk 2-6 points- 19-20% probability of PE
- High risk >6 points – 50-67% probability of PE
PESI score
|
Predictors |
Points |
|
Demographic Characteristics |
|
|
Age (yr) |
1pt/ yr |
|
Male sex |
+10 |
|
Comorbid Disease |
|
|
Cancer |
+30 |
|
Heart failure |
+10 |
|
Chronic lung disease |
+10 |
|
Clinical Findings |
|
|
Pulse >110/min |
+20 |
|
SBP <100mmHg |
+30 |
|
RR >30/min |
+20 |
|
Temp <36C |
+20 |
|
Altered Mental status |
+60 |
|
Arterial O2 sat (PaO2) <90% |
+20 |
Severity index
- The PESI score predicts 30-day all cause mortality
- Very low risk- Risk class 1 (PESI <66) = 0.8%
- Low risk- Risk class 2 (PESI 66-85) = 2.5%
- Risk class 3 (PESI 86-105) = 4.3%
- Risk class 4 (PESI 106-125) = 9.9%
- Risk class 5 (PESI >125) = 27.1%
Investigations
- FBE UEC
- D-dimer if requires as per flowchart
- ECG- looking for signs of right heart strain
- CXR to rule out other causes of chest pain or respiratory symptoms prior to CTPA
- CTPA
- Consider
- pro-thrombotic screen if PE present and unprovoked.
- troponin
Suggested medications
|
Drug |
Dose |
Frequency |
Route |
|
Paracetamol |
1g |
PRN 4hrly |
PO |
|
Oxycodone IR |
5-10mg |
PRN 4hrly |
PO |
|
Ondansetron |
4-8mg |
PRN 8hrly |
SL/ PO |
|
Metoclopramide |
10mg |
PRN 8hrly |
PO |
|
Apixaban |
|||
|
If CrCl ≥25mL/min |
5mg |
BD |
PO |
|
If CrCl <25mL/min or Any 2 of the following weight <60kg, age >80yo, Cr >133micromol/L |
2.5mg |
BD |
PO |
|
Therapeutic Enoxaparin |
|||
|
If CrCl ≥ 30mL/min |
1mg/kg |
12hrly |
SC |
|
If CrCl <30mL/min |
1mg/kg |
24hrly |
SC |
Specific observations
- Cardiac monitoring
- Report any chest pain or worsening shortness of breath to SSOU HMO.
- If chest pain present please complete ECG and
Consultations
- Discussion with haematology if PE present, patient <45yo and unprovoked PE or if pregnant
- Obstetrics if patient pregnant
Discharge criteria
- If PE present
- Low and Very Low risk PESI score
- Discharge after 4-6hours observation in ED/ SSOU total
- Ensure first dose of DOAC given in ED
- Ensure that patient is discharged with therapeutic DOAC script for 3 months
- Education / counselling for ALL patients commences on anticoagulation either via pharmacy or medical staff
- Refer to haematology clinic
- Symptoms resolved/ much improved
- Observations within normal range
- Follow-up organised
Admit to hospital if any of the following apply
- O2 required
- Submassive or massive PE present
- Troponin rise
Discharge follow-up
- GP
- Haematology if PE present and unprovoked
